Have you ever suffered such an experience: when you fall asleep, you physically act out your dreams especially the nightmares? For example, when you dream about someone chasing you, you might jump out of your bed to run away. After waking up, you could still remember the details that happened in your dream. If you are always troubled with such suffering, you probably have a REM sleep disorder.
What Is REM Sleep Disorder?
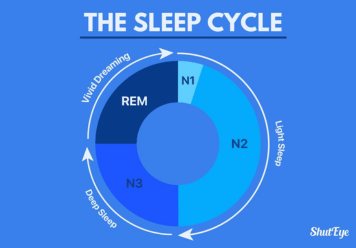
During sleep, your brain moves through several different stages. REM (Rapid Eye Movement) sleep is one of the stages of sleep cycle, in which your eyes move around rapidly in a range of directions and most of your dreams occur in this period.
REM sleep disorder refers to the sleep disorder in which you physically act out vivid, usually unpleasant dreams with vocal sounds and sudden, often violent arm and leg movements and other activity during REM sleep period — sometimes called dream-enacting behavior.
Someone with RBD (REM sleep behavior disorder) may:
- Kick, punch, flail arm, or jump from bed, in response to action-filled or violent dreams, such as being chased or defending yourself from an attack
- Create noises, such as talking, laughing, shouting, emotional outcries, or even cursing
- Be able to recall the dream if you awaken during the episode
- Conduct some sleep actions that result in an injury to them or their bed partners

How Common Is REM Sleep Behavior Disorder?
REM Sleep Behavior Disorder (RBD) is considered relatively rare compared to other sleep disorders. Estimates suggest that it affects about 0.5% to 2% of the general population. However, its prevalence may be higher in certain groups, such as older adults or individuals with neurological conditions like Parkinson’s disease or multiple system atrophy. Additionally, RBD tends to be more common in men than in women. Despite its relatively low prevalence, REM Sleep Behavior Disorder can have significant impacts on an individual’s quality of life and may require medical intervention to manage symptoms effectively.
What Causes REM Sleep Disorder?
The exact cause of RBD is unknown. Animal studies suggest that it has to do with certain neural pathways in the brain. During normal REM, nerve pathways in the brain that prevents muscles from moving are active, which could keep your body temporarily “paralysis”. However, with RBD, these pathways might no longer work and you may physically act out your dreams.
Risk factors for RBD may include:
- Being male and over 50 years old
- Some neurological disorders, like Parkinson’s disease, Lewy body dementia, or multiple system atrophy
- Sleep or REM sleep deprivation
- Other sleep disorders (such as narcolepsy)
- Use or withdrawal from drugs, such as CBD or alcohol
- Some antidepressants, including tricyclic antidepressants and serotonin-specific reuptake inhibitors.

Symptoms of REM Sleep Behavior Disorder
During episodes of REM Sleep Behavior Disorder, you may exhibit physical actions such as kicking or punching during your dreams. Here are three common symptoms to help you understand this disorder better:
- Lack of temporary paralysis during REM sleep.
- Physical actions like kicking or punching during dreams.
- Noises such as talking or shouting may accompany actions.
If you wake up during an episode, you might recall your dreams vividly. Remember, these symptoms can worsen over time, so seeking medical advice is crucial for proper diagnosis and treatment of REM sleep behavior disorder.
If you or someone you know experiences these behaviors during sleep, consult a healthcare provider for guidance on managing REM Sleep Behavior Disorder effectively.
Complications Of Rem Sleep Disorder
REM Sleep Behavior Disorder (RBD) can lead to various complications, both for the individual experiencing the disorder and potentially for their sleep partners or others nearby. Some of the complications include:
- Injury: Individuals with RBD may act out their dreams violently, leading to self-injury or injury to their sleep partners. They may punch, kick, or thrash about during episodes of REM stage of sleep, potentially causing bruises, cuts, or other injuries.
- Sleep disruption: RBD can disrupt the sleep of both the affected individual and their sleep partner. Episodes of acting out dreams can lead to frequent awakenings during the night, resulting in fragmented sleep and daytime sleepiness.
- Emotional distress: Experiencing vivid and often intense dreams during RBD episodes can be emotionally distressing for individuals. They may feel confused, frightened, or embarrassed by their behaviors during sleep.
- Relationship strain: The disruptive nature of RBD episodes can strain relationships, particularly if sleep partners are frequently disturbed or injured during the night. This can lead to tension, resentment, or sleep disturbances for both parties.
- Increased risk of accidents: Daytime sleepiness resulting from disrupted sleep in RBD can increase the risk of accidents or errors during daily activities, such as driving or operating machinery.
- Underlying medical conditions: RBD is associated with an increased risk of developing certain neurological conditions, such as Parkinson’s disease or other neurodegenerative disorders. Identifying and managing RBD may be important for detecting these conditions early and initiating appropriate treatment.
Overall, the complications of RBD highlight the importance of seeking medical evaluation and treatment for individuals experiencing symptoms of the disorder. Management strategies may include lifestyle modifications, medication, or other interventions aimed at reducing the frequency and severity of RBD episodes and improving overall sleep quality and safety.
Related content:
REM Sleep Behavior Disorder Diagnosis
Diagnosing REM Sleep Behavior Disorder (RBD) involves several steps:
- Clinical evaluation: A healthcare provider assesses symptoms, medical history, and sleep patterns, focusing on unusual behaviors during sleep like acting out dreams.
- Sleep study (Polysomnography): This comprehensive test monitors various sleep parameters, identifying abnormalities in REM sleep, such as the absence of muscle paralysis.
- Video recording: Video during sleep complements polysomnography, visually capturing any abnormal behaviors during REM sleep, aiding in diagnosis.
- Exclusion of other conditions: Healthcare providers rule out sleepwalking, nocturnal seizures, or other parasomnias that mimic RBD, ensuring an accurate diagnosis of REM Sleep Behavior Disorder.
- Evaluation for underlying conditions: Further assessment for neurological disorders associated with RBD, like Parkinson’s disease, may be needed.
A team approach involving sleep specialists, neurologists, and other healthcare providers ensures accurate diagnosis and appropriate management. Early detection and intervention are crucial for improving outcomes and reducing complications.
Treatments for REM Sleep Behavior Disorder
The treatment for it is tailored to an individual and may involve a combination of lifestyle changes and medication.
1. Lifestyle changes
A good lifestyle is conducive to improving the quality of sleep and decreasing the risk of suffering RBD.
There are some tips for you:
- Maintain a consistent and healthy sleep schedule
- Avoid certain medications and alcohol
- Regular monitor your sleep conditions by some sleep apps (such as ShutEye®)
- Creating a safe sleeping environment for avoiding any injury caused by RBD

2. Medication
A number of medications have proven effective in cases of RBD depending on which symptoms present. Currently, two main drugs are used to effectively treat RBD including melatonin and clonazepam.

Before taking any medication, you’d better consult a doctor. They can best advise you on a treatment plan based on your medical history and symptoms.
If you believe you or your loved one may have REM sleep behavior disorder, it is best to tell your doctor.
To sum up, the REM sleep disorder is a condition in which a person can not completely shut down muscle movement and performs the action in their dreams.
Though it is relatively uncommon in our life, it is associated closely with our sleep quality, which should not be ignored. By adopting proper treatment including lifestyle adjustments and medication, we could reduce the potential risk of suffering this sleep disorder and the injury it might cause.
Pathophysiology and Etiology
The pathophysiology of REM Sleep Behavior Disorder involves abnormalities in dopaminergic function. In individuals with RBD, dopaminergic abnormalities have been observed, suggesting a role for dopamine in the regulation of REM sleep.
Additionally, lesions in the pons region of the brain can lead to synucleinopathies and the manifestation of RBD symptoms. Progressive degeneration of specific nuclei in the pons may contribute to the development of RBD, potentially explaining the disorder’s association with neurodegenerative conditions like Parkinson’s disease.
This failure of inhibitory mechanisms during REM sleep results in the physical acting out of dreams characteristic of RBD. Understanding these underlying abnormalities is crucial for diagnosing and managing REM Sleep Behavior Disorder effectively.
Conclusion
In conclusion, REM Sleep Behavior Disorder can cause disruptive and potentially dangerous behaviors during sleep due to the lack of muscle paralysis. Early diagnosis and treatment are crucial to manage the symptoms and prevent complications.
By understanding the symptoms, causes, and treatment options for this disorder, individuals can effectively manage their condition and improve their quality of sleep. Remember to consult with a healthcare provider if you suspect you may have REM Sleep Behavior Disorder.
You may also like:
Are You Stressed? | 3-Minute Stress Test
14 Sleep Hygiene Tips For Better Sleep
8 Relaxing Sounds to Help You Sleep Better and Relieve Stress